Rachel S. Bensman, MD
Airway management in pediatric arrest
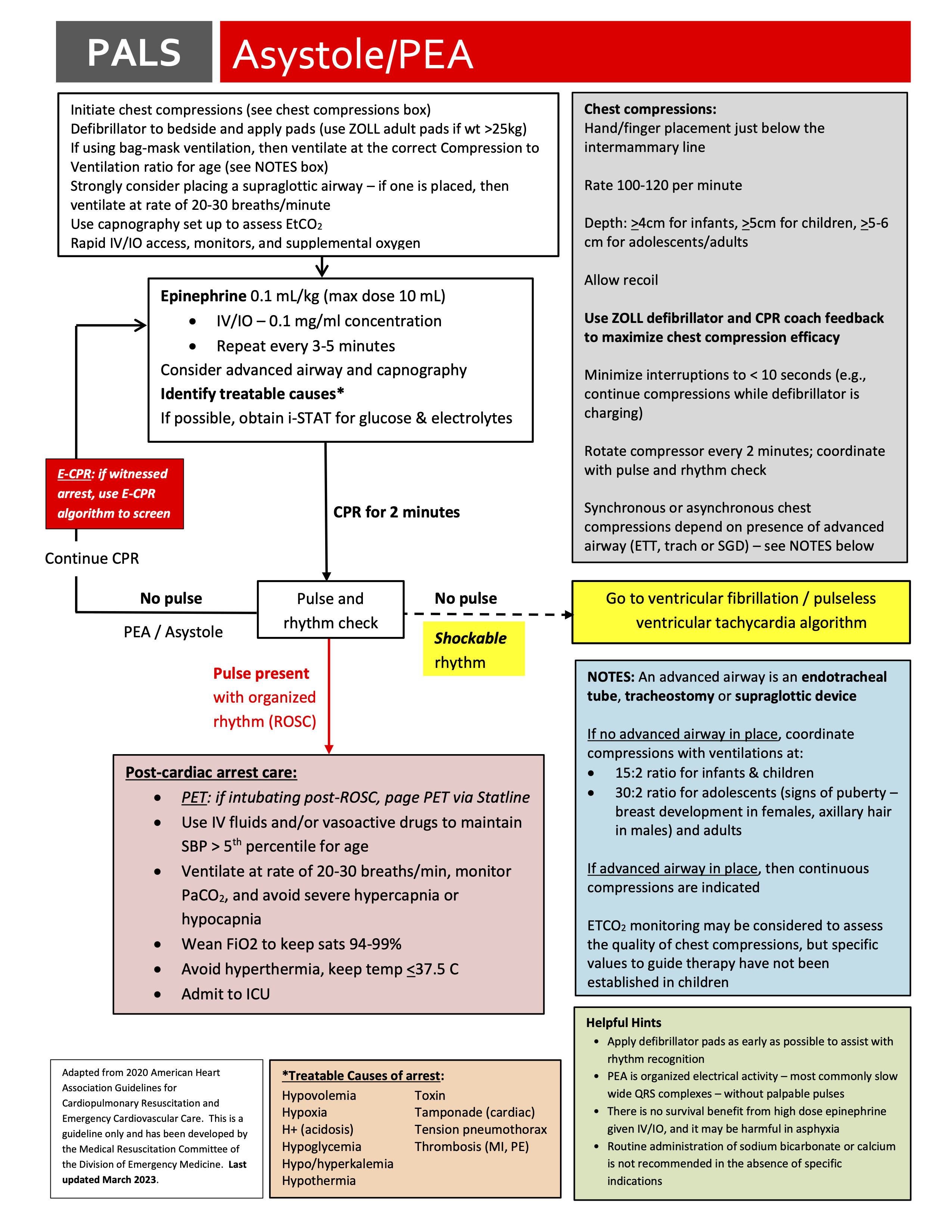
For patients in cardiac arrest, we recommend early placement of a supraglottic airway (SGA, for most patients the Igel) with immediate continuous capnography to assess placement of the SGA and effectiveness of ventilations.
In its 2020 update on advanced life support, the American Heart Association states that bag-mask ventilation (BMV) is a reasonable altyernative to SGA and endotracheal intubation (ETI) for children in cardiac arrest. This recommendation is based on low-quality or limited evidence in children. The AHA does list three reasons why an SGA might be preferred: (1) some evidence of improved return of spontaneous circulation, (2) more stable and reliable airway control, and (3) lower risk of aspiration. However, there are no randomized controlled trials comparing endotracheal intubation (ETI) to SGA in pediatric arrest. Although adjusting for all confounding variables is difficult, observational studies have shown that ETI during pediatric in-hospital cardiac arrest is associated with no benefit or even decreased survival (Anderson et al, 2016) compared to SGA or BVM. A meta-analysis of both in and out-of-hospital cardiac arrest demonstrated no outcome differences for ETI vs SGA (Lavonas et al, 2019). In adults, a recent meta-analysis in adults with out-of-hospital arrest showed that SGA was superior to ETI and BMV for ROSC but not survival (Wang et al, 2020). There have been 2 large RCTs for advanced airway management in adults with out-of-hospital cardiac arrest (both included in the meta-analysis):
- The PART trial found improved survival and favorable neurologic status with laryngeal tube (eg, King) vs ETI (Wang et al, 2018).
- The AIRWAYS-2 trial found improved initial ventilation success rates with SGA vs ETI, but no difference in other outcomes (Benger et al, 2018).
