Key Literature
Kerrey et al. Rapid Sequence Intubation for Pediatric Emergency Patients: Higher Frequency of Failed Attempts and Adverse Events Found by Video Review, Annals of Emergency Medicine 2012.
Publication summary: The limited literature on emergency pediatric intubation, which generally relies on chart review of self-report, suggested the procedure was safe and successful for the majority of patients. Using the video-review system in our resuscitation area, from we studied pediatric patients undergoing rapid sequence intubation (RSI) over 12-months (2009-10) in one pediatric emergency department. Video review revealed that first pass success was close to 50% and more than 25% of patients required 3 or more attempts. Prolonged attempts were common, with many lasting more than 60 seconds. Adverse events were also common, with more than 60% of patients experiencing at least one. 33% of patients had at least one episode of oxyhemoglobin desaturation during RSI, most of which were severe (<70%). Two patients developed cardiac arrest during RSI. The study has been cited more than 120 times since publication and inspired several similar studies at other centers.
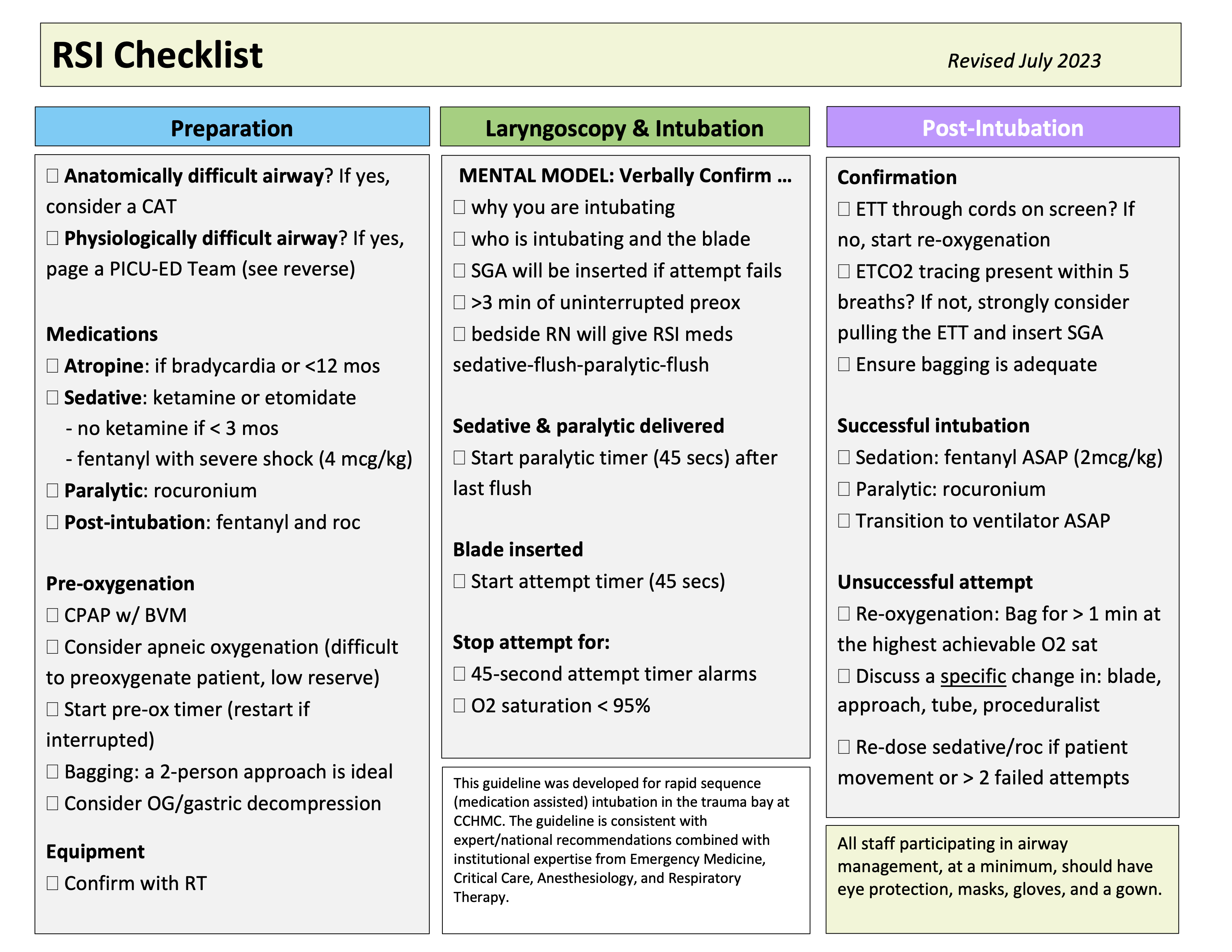
What this Work Produced: This initial RSI study was the first of numerous emergency airway management/video-based studies over the last 10 years. This work has spanned the spectrum of scientific investigation, from knowledge generation to translation and quality improvement. In 2013, we completed a successful RSI improvement initiative, raising our first pass success to 70% and reducing the percentage of patients with desaturation during RSI to 20%. We dramatically reduced the occurrence of multiple desaturation events, prolonged attempts, and esophageal intubation. Importantly, we have continued to monitor performance of RSI in our PED, collecting data on all cases by video review. This work has also led directly to the development of two other airway management programs – the Critical Airway Team (CAT) and the PICU-ED Team (PET). We have also established a video-based living lab for airway and other resuscitation research and co-founded the multicenter Videography In Pediatric Emergency Research (VIPER) collaborative. Finally, our video-based program supports numerous peer review and quality assurance activities and has been used by numerous fellows and trainees in their scholarly and academic work.
